My digital twin in the podcast: A look at fall risks based on real-world data

I have a very specialpodcast to tell you about today. My digital twin, created withNotebookLM from Google, has recorded a podcast for me.
And the topic is no less exciting: it's about our latestpublication, which is based onreal-world data and thecorrelation between fall risk and actualfalls in older adults.
Imagine we're moving as a company, unpacking the boxes, setting up the desks - and a podcast on a deeply technical topic is being created along the way. Because the renownedJMIR Aging Journal (Impact Factor 5.0) has published our submission:
"Evaluating the prognostic and clinical validity of the Fall Risk Scorederived from an AI-based mHealth application for fall prevention: a retrospective real-world data analysis"
What's so special about this podcast?
My digital twin sat down with one of the authors of the World Fall Guidelines, a globally recognized expert on fall prevention, and discussed my recently published study on fall risk assessment.
In the study, we examined an artificial intelligence-based mHealth application (LINDERA Mobility Analysis) for fall prevention.
The app was used in German care facilities and calculates afall risk score(FRS).
The special feature: the app records the user's gait parameters via a smartphone-based video analysis and records additional risk factors using a questionnaire.
The rejection shows once again that the care sector cannot be assessed using criteria from the field of pharmacology. Simply looking at scientific evidence without incorporating nursing expertise leaves no room for the realities of everyday nursing care.
In nursing practice, there are unavoidable influencing factors that cannot be fully taken into account in scientific study designs.
At the same time, the urgency to find innovative solutions for care remains unaffected - because the number of fatal falls at home has doubled in the last ten years according to the NRW State Statistical Office.
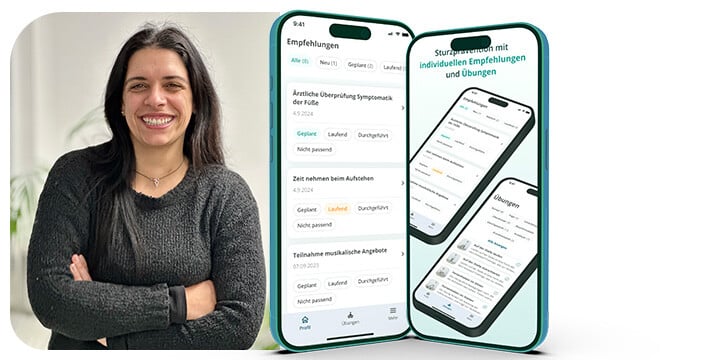
Screenshots of mHealth-Application
The podcast focuses entirely on the validity of the FRS and its practical application. My digital twin and the World Fall Guidelines expert present the app in detail and explain its functions.
They then discuss the correlation between FRS and actual falls. This highlights the significance of these findings for fall prevention.
Next, they explore the Minimum Clinically Important Differences (MCIDs) for FRS changes. MCIDs help clinicians assess whether a change in FRS following an intervention, such as a training program, is actually clinically relevant.
An example: If someone changes their FRS by more than the MCID value of 2.3 during assessments, for instance from 35 to 32, we can say that this change makes a difference in fall risk.
Furthermore, the study also identified threshold values for the FRS.
These thresholds indicate at what FRS level the risk of a fall within a specific timeframe significantly increases.
For example, an FRS above 45% means there is an increased risk of falling within six months.
The combination of thresholds and MCIDs provides a valuable foundation for planning and evaluating fall prevention measures.
Special Risk Groups
I found the discussion about subgroup analysis particularly interesting, where significant correlations between fall risk and falls were identified.
Various factors were considered, including age, fall history, dementia, gait speed, and the use of walking aids.
The study showed that, for example, slower gait speeds and the use of walking aids demonstrate a significant association between fall risk and actual falls.
These findings help identify which patient groups are at higher risk. Particularly patients with slowed gait or those dependent on walking aids may require more intensive monitoring and preventive fall prevention measures.
Fall Prevention in Focus: Human Needs First
mHealth applications like the one we studied can meaningfully complement fall prevention.
However, it's important to understand the limitations of technology and always interpret results in individual context.
Person-centered fall prevention, as recommended by the World Fall Guidelines, must always take priority.
Heartfelt thanks go to all co-authors (Steffen Temme, Seyedamirhosein Motamedi, Marie Kura, Sebastian Weber, Johannes Zeichen, Wolfgang Pommer, André Baumgart) and especially to the 617 patients who enabled the use of their data and thus made this study possible.
I warmly invite you to listen to the podcast and form your own opinion about the study.
The connection to nursing practice can be found in our press release.